This is a story about an anniversary, which occurred today, and a single day on a bike, which occurred three days ago. I hope you get something out of it because I did and I think the thoughts and experiences are worth sharing.
Today, July 22, 2014, is the five year anniversary of my double spinal fusion surgery at L4-L5 and L5-S1, which is why I wear a CamelBak even on a road bike. L4-L5 and L5-S1 are the two lowest vertebrae in your back. I like to say that I was screwed five times in one day, and I can prove it. Prior the day of the surgery, I could not get my own socks on or off or tie my own shoes.
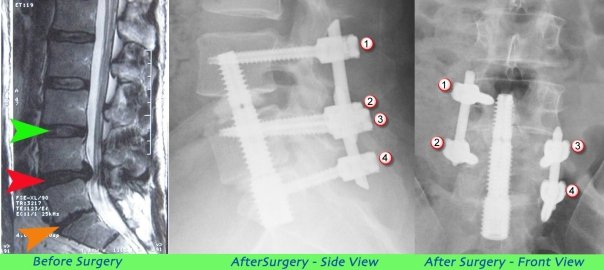
The left side shows the herniation of L4-L5, and the collapse of L5-S1. The middle and right images are the spinal fusion screws.
I was an avid cyclist before my back was injured, which originally occurred when I was rear ended by a van while riding my bike. I was thrown of the bike onto the sidewalk and slid over 20 feet before coming to a stop right before a concrete light pole. That accident eventually led to a microdiscectomy at L5-S1 in 1999, and I was fine after that procedure. Then, in 2007, I was driving my car with my daughter in the back seat when a driver ran a red light and hit us as I was turning. That led to the double spinal fusion and I stopped riding my bike for several years until I caught the “bike bug” again at the end of October 2013. It felt great to be back on the bike but I was hit again by a driver who made an illegal U-turn when I was traveling straight in December 2013. I have never needed my bike helmet like I needed it that day, which was also on the 22nd of the month. My head bounced off the street after I ran straight into the car’s driver side rear door. I have always said, “there is only one reason to wear a helmet, which is if you have a brain,” and I basically walked away from that accident with sore ribs, some back pain for a few months, and a scar on my right knee.
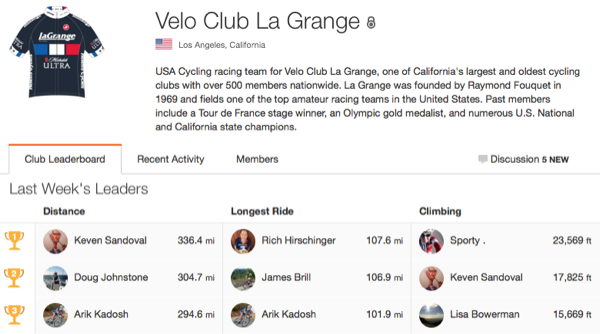
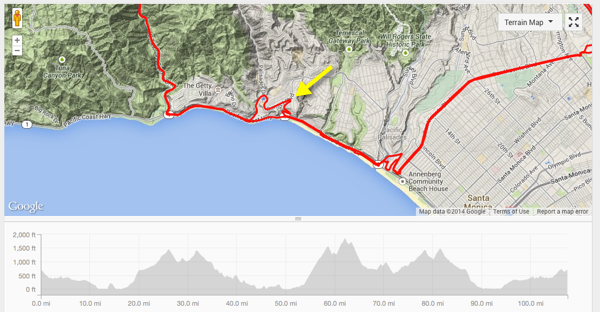
After I recovered from that accident, I started riding even more. I rode my longest ride ever, a 117 mile journey from Los Angeles to the campus at UCSB to visit my daughter who was finishing her first year in college. That ride was six days before the murder rampage in Isla Vista that took the lives of six UCSB students. This past Saturday, one of my friends in Velo Club La Grange, which is my local cycling club, wanted to go on a long ride with a lot of vertical climbing. The ride ended up being over 107 miles long with over 9,000 feet of climbing but it is what happened on the ride that is important. I use Strava, which lets you track your activities along with your friends activities, and I was very surprised that I had the longest ride of the week last week for my cycling club, which is something I would not have envisioned five months ago let alone five years ago.
About 12 miles into the ride, we had to take a detour on Pacific Coast Highway (PCH) since the road was closed due to a very tragic decision a young lady made. Those of you that ride PCH in Santa Monica will notice the squiggly line indicated by the yellow arrow on the map below, which is the detour we had to take through the Bel Air Bay Club up to Sunset and then back down to PCH.
The young woman, who was in her 20’s, tried to cross PCH at 3:30 a.m. That was likely the second to last thought she had since she was hit by a car, which is why the road was closed. She died from her injuries the same day. It was not lost on me the split second decisions we make during our lifetime, which in this case, was a fatal decision. Take the time to really think your decisions through. Some thoughts are not work the risk.
From PCH we climbed up Topanga Canyon to Mulholland Drive then back to PCH via Malibu Canyon, then back up to Mulholland via Encinal Canyon. At Mulholland and Malibu Canyon, which was at mile 72 give or take a few tenths of a mile, my friend saw one of his friends on the side of the road with a flat tire. We stopped to help, and coincidentally there was a NBC News reporter interviewing a cyclist about a video rant that had been posted online by a reserve police officer for the Santa Paula Police Department. The video was about how much she hated cyclists, and how much the driver of the car she was in would charge to run them over. Some people think this is merely freedom of speech. Others think it is very disturbing that anyone, let alone an officer of the law, would suggest running over cyclists with a car.
Jane Yamamoto was the NBC News reporter who interviewed me as well as a few other cyclists to get our opinion on the video, which you can watch below.
The decision made by the reserve police officer to post her video took several hours since the video had to be conceived, filmed, edited, and then posted. It was not a split second decision. But the decision cost her her job since the Court of Public Opinion convicted her of horrendously poor judgment, and she ended up resigning from her position. What astounded me is that she is a personal trainer yet she hates cyclists even though they are outside exercising, which is what she has her clients do for a living.
I’m very happy with the decision I made five years ago to have my back surgery done. Some people question my decision to continue to ride my bike since I have been hit by a vehicle twice. I feel good about my decision since riding my bike makes me feel alive, and we have to live when we are above ground. Take the time to make good decisions in your life. Quick decisions can cost you your life, and other decisions that you think are the right decision at the time can turn out to cost you as well.
Lastly, don’t make excuses for why you can’t do something. The mind is a very powerful tool. You can talk yourself into not doing something or you can talk yourself into doing something. Anything worthwhile is going to be hard work. Which is why work is a four letter word. Be safe, have fun, and take advantage of the time you have. It is a very precious gift.