I am a Board-certified orofacial pain specialist. It is a unique specialty of dentistry, which I learned during a two-year residency at the UCLA School of Dentistry Orofacial Pain and Dental Sleep Medicine program. I am now a clinic-co-Director of the UCLA residency one day a week and I have a private practice in Beverly Hills, CA the other four days of the week. I have been treating patients who complain of “TMJ” for the past 7 years and I never need to touch teeth since my training proved to me that the pain patients complain about are not related to occlusion, which is how teeth meet. If it is not related to the bite, what is it related to? I would say the 98% of the patients who think they have pain related to their TMJ, are actually suffering mainly from muscle pain. The pain is mainly due to overuse of the muscles from daytime clenching and/or bad oral habits during the day such as chewing gum, nail biting, and nighttime habits such as clenching and/or grinding during sleep. Any muscle that gets over used needs a break. If the muscles do not get a rest, they will start causing pain.
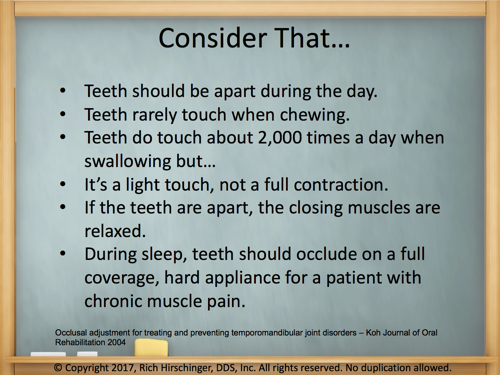
There are four muscles that close the jaw. These muscles are the superficial masseter, deep masseter, temporalis, and medial pterygoid. The superficial masseter, when measured on a pounds per square inch basis, is the strongest muscle in the human body. When patients come into my office I always have them point with one finger where their main pain is and they almost always point to the angle of the jaw, which is the superficial masseter. When your teeth are touching, the closing muscles of the jaw are contracted. As humans, we do not walk around with our teeth together. If you find yourself clenching your teeth during the day, you need to stop. Your teeth should be apart during the day in the “N-Rest” position, which you can learn about at this page on my website. The graphic below is from a slide I give to dentists and other specialists that want to learn what I do.
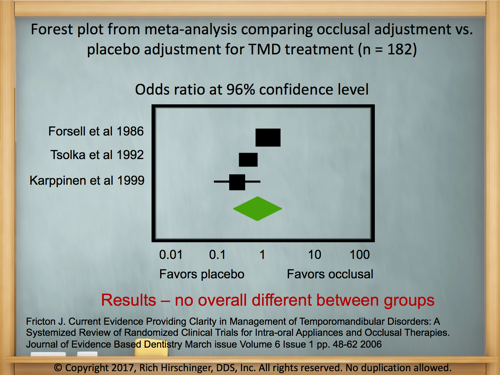
You don’t have to just take my word for it. My training is evidence-based. A fantastic paper by Dr. James Fricton showed that a placebo equilibration is slightly better than an occlusal equilibration. What does this mean? An occlusal equilibration is an irreversible surgical procedure where a dentist grinds a small amount of enamel off your teeth or material off your crowns, fillings, etc. to get your teeth to meet more evenly. However, Dr. Fricton’s paper showed the when you do a placebo equilibration that patients report more improvement. A placebo equilibration is when the patient thinks their bite was adjusted when in reality nothing was done. This is accomplished by “adjusting” the teeth with the smooth end of a dental bur. The patient thinks something was done since they felt the vibration of the drill on their teeth but in reality, nothing was adjusted.
The bottom line is this. It is incumbent upon all health care providers to try all non-surgical and reversible procedures first before doing surgery. Cutting healthy teeth or existing crowns or fillings is surgery and it is not reversible. If you suffer from what you think is TMJ, try softening your diet, keep your teeth apart during the day, stretch your jaw muscles several times a day, and during sleep wear a hard, full coverage night guard preferably over your lower teeth. I never have patients wear an appliance 24 hours a day, I never have patients wear an appliance during the day, and I never have patients wear an appliance for “TMJ” that is designed to change their bite. If your dentist ever uses the terms “Phase 1 and phase 2,” I would highly encourage you to get a second opinion from a Board Certified specialist in orofacial pain. Here is a link to the American Board of Orofacial Pain member directory. I would be happy to see you at my office in Beverly Hills if you are in the Los Angeles area. Remember, it is not about the bite. It is about keeping your teeth apart.
References:
Fricton J. Current Evidence Providing Clarity in Management of Temporomandibular Disorders: A Systemized Review of Randomized Clinical Trials for Intra-oral Appliances and Occlusal Therapies. Journal of Evidence Based Dentistry March issue Volume 6 Issue 1 pp. 48-62 2006
Occlusal adjustment for treating and preventing temporomandibular joint disorders – Koh Journal of Oral Rehabilitation 2004
Temporomandibular disorders and dental occlusion. A systematic review of association studies: end of an era? – Journal of Oral Rehabilitation Volume 44, Issue 11, pages 908–923, November 2017










 Fold the range of motion scale in half at the black triangle on the lateral scale. Measure the overjet, then ask the patient to move their jaw forward “like a bulldog” and measure that number. Record those two numbers as separate numbers such as “2+8” so that you know the overjet plus how far they can protrude forward from their centric occlusion.
Fold the range of motion scale in half at the black triangle on the lateral scale. Measure the overjet, then ask the patient to move their jaw forward “like a bulldog” and measure that number. Record those two numbers as separate numbers such as “2+8” so that you know the overjet plus how far they can protrude forward from their centric occlusion.
