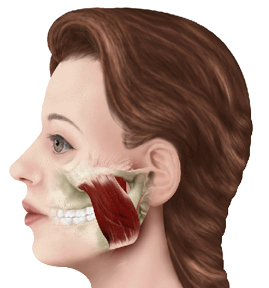
Headaches Explained by Dr. Rich Hirschinger Beverly Hills
I learned very early in the first few days of my two year orofacial pain residency at UCLA that “headache is not a diagnosis.” Every time I make a diagnosis of a type of headache it is based on the criteria of the International Headache Society. This post will help you understand what type of headache you might have and will focus primarily on migraines.
It is very important to understand the difference between a primary headache, and a secondary headache. A primary headache is a headache that is not attributed to another disorder. A secondary headache is a headache that is attributed to another disorder such as a tumor, a stroke, a brain bleed, etc. In other words, there is nothing else causing a primary headache whereas a secondary headache is caused by something else.
I use several acronyms to remember the various types of headaches, some of which I learned from others and a few that I created myself. One of the acronyms I learned from others is SNOOPS. These are the “red flag” signs of headaches that require immediate attention.
S stands for systemic, which include symptoms such as a fever, and weight loss.
N stands for neurological, which includes symptoms such as confusion, altered level of consciousness, or numbness.
O stands for onset such as a very sudden, abrupt, split second onset of the headache.
O stands for older. If you are older than approximately 50 years of age, and the headache is a new onset or progressive, that is a red flag.
P stands for previous history of headaches. If you have a previous history of a headache but this headache is new or different, if there is a change in attack frequency, severity or clinical features then that is a red flag.
S stands for secondary risk factors. If you have a systemic condition such as HIV, or systemic cancer along with the headache that is a red flag.
If you have any of these red flags, immediate attention in an emergency room is the best course of action.
Primary Headaches
There are four categories of primary headaches, which are:
- Migraine
- Tension-type headaches
- Cluster headache and other trigeminal autonomic cephalalgias
- Other primary headaches
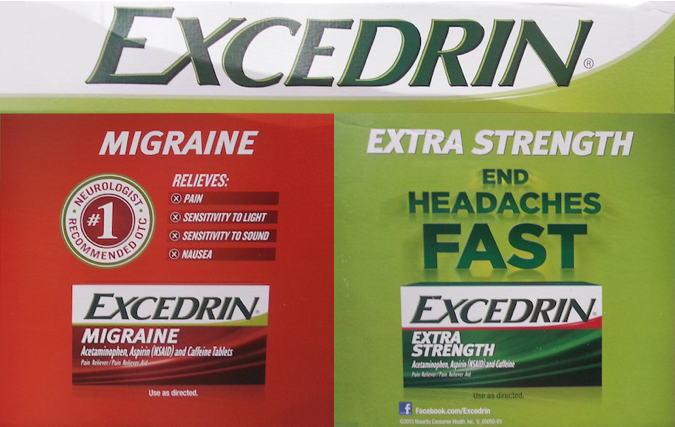
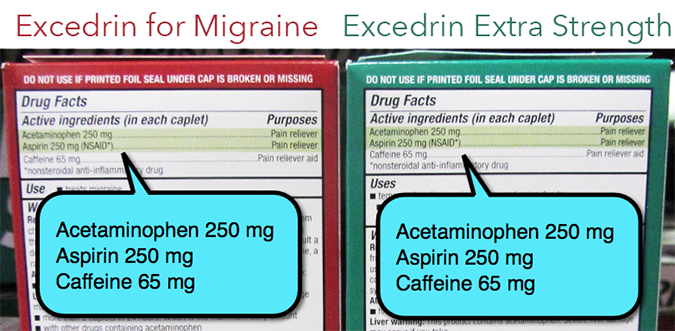
Migraine

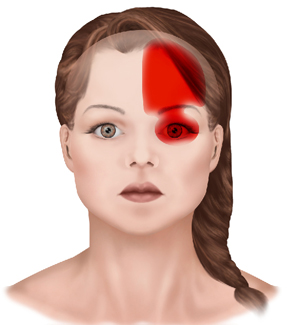
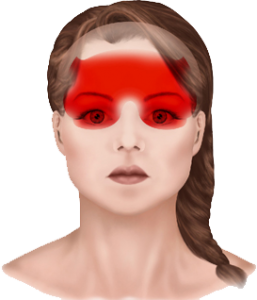
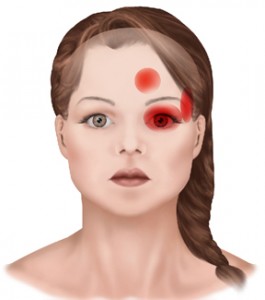
Over 60% of migraines are unilateral
There are many types of migraine headaches but the main type of migraine headache is easy to diagnose based on the International Headache Society criteria. The acronym I created to remember the criteria is 5472 PUMA PPNV ACE. Let me explain how to interpret the acronym so that it makes sense.
Many people think that since they have a headache it is a migraine. This could not be further from the truth. Just like headache is a not a diagnosis, if you have a headache, it does not necessarily mean you have migraines. If you meet the following criteria, then you have a migraine.
Migraine Criteria 5472 PUMA PPNV ACE
5472 – If you have had 5 headaches in your life lasting between 4 and 72 hours that was untreated or did not respond to treatment, then move to the next set of criteria to see if you have a migraine headache.
PUMA – If you have two of the four PUMA criteria during the headache, then move to the next criteria to see if you have a migraine headache.
- P stands for pulsating, throbbing type of headache.
- U stands for unilateral. Over 60% of migraines are unilateral, which means a one sided headache.
- M stands for moderate to severe.
- A stands for aggravation with exertion meaning the headache gets worse if you walk, run, work out or exert yourself.
PPNV – If you have one of the following criteria during the headache, including the above criteria, then you have met the diagnosis of a migraine.
- Photophobia and phonophobia. Photophobia means that the headache causes you to be sensitive to light, and phonophobia means that the headache causes you to be sensitive to sound.
- Nausea and/or vomiting.
ACE – If the criteria for migraine has been met then ask if there is an aura, and how frequent the migraine headaches occur.
A stands for aura. Aura’s can be positive or negative, and they can be visual or sensory, and the symptoms are completely reversible.
C stands for chronic. If you get 15 or more migraines a month, it is a chronic migraine.
E stands for episodic. If you get less than 15 migraines a month, it is an episodic migraine.
Aura – An aura gradually develops over a period of about 5-20 minutes and lasts for less than an hour.The aura can be fully reversible visual symptoms like lines, spots, or beautiful colors, which are all positive auras meaning you see something extra, or holes in the visual field called scotomas, or gray spots, which are all negative auras meaning you see something less than you usually see. The aura can also be fully reversible sensory symptoms such as like pins and needles, or numbness, which is a positive aura, or slurred speech, which is a negative aura.
Based on the above criteria, you should be able to know if you truly suffer from migraines. In the next post, I will discuss how to treat migraines, which is based on both abortive treatments, meaning how to treat the migraine after it starts, and preventative treatments, meaning how to help prevent migraines from occurring.
Quick Migraine Symptom Diagnosis
Having stated all of the above, research shows a very simple way to determine if you have a migraine by answering the following questions.
- Has the headache limited your activities for a day or more in the last three months?
- Are you nauseated or sick to your stomach when you have a headache?
- Does light bother you when you have a headache?
Patients who answer positively to two out of these three symptom questions have a 93% chance of a migraine diagnosis and, if all three are answered positively, a 98% chance of a migraine diagnosis. If think you have a migraine, or if you know you have migraines but the previous treatments have not been helpful, you can request an appointment at my Beverly Hills migraine headache office. As always, I’m happy to try to answer any questions you might have.
Respectfully,
Rich Hirschinger, DDS, MBA
Diplomate, American Board of Orofacial Pain
Member American Academy of Orofacial Pain
Lecturer, UCLA Orofacial Pain and Dental Sleep Medicine
www.LoveOFP.com
888.981.8981
 ing involved in a bike accident, any layman can do a quick assessment of the injured person to check for a sign of a possible brain concussion.
ing involved in a bike accident, any layman can do a quick assessment of the injured person to check for a sign of a possible brain concussion.