Diplomate American Board of Orofacial Pain
9615 Brighton Way, Suite 323
Beverly Hills, CA 90210
888.981.8981
Sphenopalatine Ganglion Blocks
A sphenopalatine ganglion (SPG) block is a medical procedure used to manage certain types of head and facial pain by delivering anesthetic to the sphenopalatine ganglion, a nerve cluster located in the pterygopalatine fossa behind the middle nasal turbinate.
What is the SPG?
The sphenopalatine ganglion is a parasympathetic ganglion associated with the facial nerve (CN VII). It also receives sensory input from the maxillary nerve (V2), which is a branch of the trigeminal nerve (CN V), and sympathetic fibers from the deep petrosal nerve. It plays a key role in:
- Lacrimation (tear production)
- Nasal secretions
- Vasodilation of cerebral and meningeal vessels
What is an SPG block?
An SPG block involves applying local anesthetic to the area around the SPG to interrupt pain signals and modulate autonomic activity. The procedure takes about 20 minutes. Ten of those minutes are spent lying flat with your head tilted back.
Indications:
Cluster headaches
Migraine (including status migrainosus)
Trigeminal autonomic cephalalgias (TACs)
Atypical facial pain
Postherpetic neuralgia
Temporomandibular joint disorder (less common)
Routes of administration:
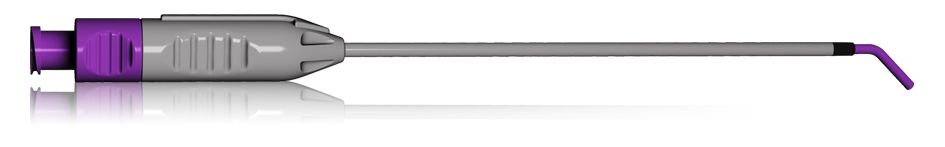
Transnasal (most common) – cotton-tipped applicator or catheter with anesthetic inserted through the nostril. Dr. Hirschinger uses this approach using a Sphenocath, which is shown in the image below. It is not an injection, and there is no skin broken and no bleeding. Each administration takes about 20 seconds per nostril. Viscous lidocaine is pushed through the Sphenocath.
Transoral – through the greater palatine foramen
Lateral infratemporal approach – image-guided injection via needle
Effects:
Interrupts parasympathetic outflow and sensory input to reduce vasodilation and inflammation
Can provide rapid pain relief, sometimes within minutes
May be diagnostic and therapeutic — i.e., a positive response can guide further treatment
Risks:
Minimal with transnasal approach
Possible side effects:
Numbness in throat, bitter taste, nosebleed, dizziness, rarely infection or local trauma